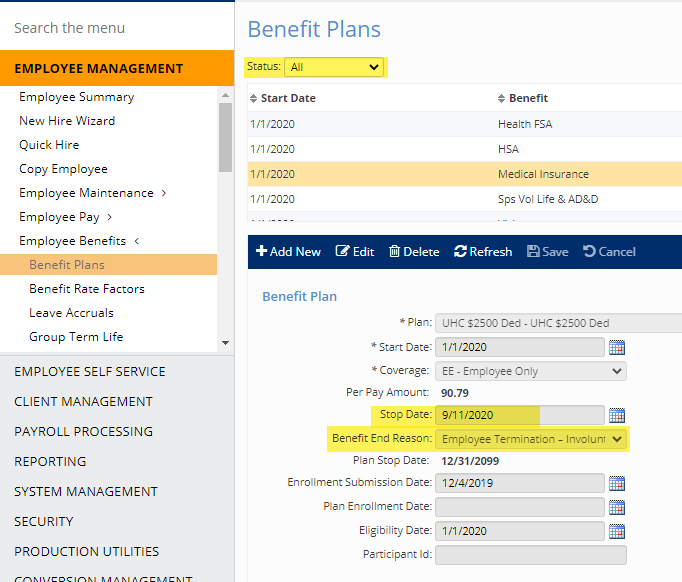
The first step to ensure COBRA documents were transmitted correctly is to make sure all cobra eligible benefits are terminated in isolved and have a benefit end reason listed. To do this follow the trail below:
Select the Employee > Employee Management > Employee Benefits > Benefit Plans. Change status drop down to “All”.
Make sure COBRA eligible plans (medical, dental, vision) have a stop date populated and that the Benefit End Reason is populated.
If the plan is terminated and the benefit end reason is populated, the COBRA notices should have transmitted.
If for any reason the documents were not received by the employee as expected then they can contact Infinisource directly or visit the portal.
This contact information can be found in isolved under “My Account Reps”.
